HSDD
What is HSDD?
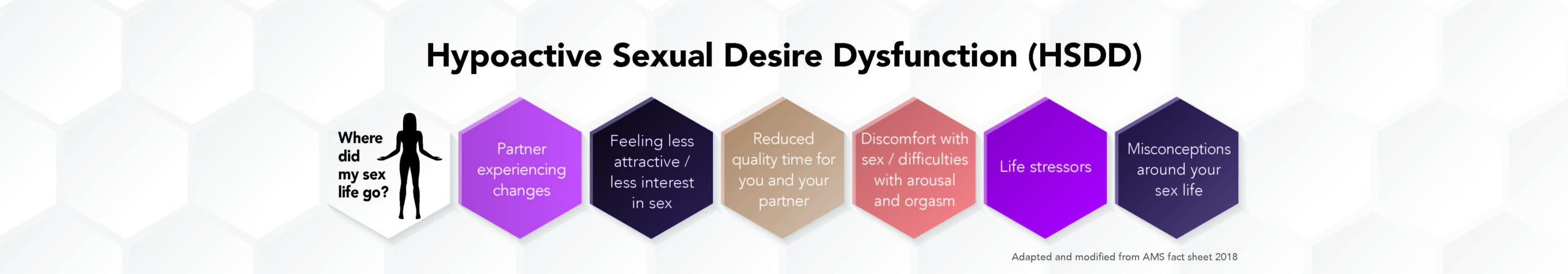
Hypoactive sexual desire dysfunction (HSDD) is an extremely common medical condition that causes distress resulting from a low sexual desire.
It manifests as any of the following:
- the absence of spontaneous sexual desire (sexual thoughts, fantasies, stimulation)
- lack of desire to initiate or participate in sexual activity
- significant personal distress such as feelings of frustration, grief, incompetence, loss, sadness, sorrow, or worry1
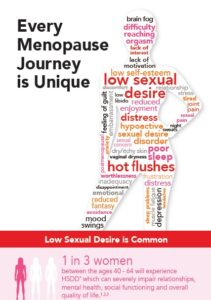
Clinical data indicates that 7 in 10 women (aged 40-64) presented with low sexual desire, and 1 in 3 women (aged 40-64) reported low desire with distress (HSDD)2.
The prevalence of HSDD was even significantly greater among younger surgically postmenopausal aged 20 – 49.3
- The International Society for the Study of Women’s Sexual Health Process of Care for Management of Hypoactive Sexual Desire Disorder in Women – Clayton A et al. Mayo Clinic Proceedings 2018 93(4):467-487
- Prevalence and Predictors of Low Sexual Desire, Sexually Related Personal Distress, and Hypoactive Sexual Desire Dysfunction in a Community-Based Sample of Midlife Women J Sex Med Worsley R et al. J Sex Med 14:675-686
- Hypoactive sexual desire disorder in postmenopausal women: US results from the Women’s International Study of Health and Sexuality (WISHeS) Leiblum SR et al. Menopause 2006;13(1):46-56
Symptoms
Do any of the following resonate with you?
- I want sex much less than my partner and it’s causing distress in our relationship
- I have no interest in any sexual activity with my partner
- I have no interest in masturbation
- I rarely have sexual thoughts or fantasies
- I’m concerned about my lack of sex drive
Possible Causes
- Medical: many underlying conditions can contribute to HSDD including hypertension, coronary artery disease, diabetes, hypothyroidism, urinary incontinence, gynaecologic conditions (uterine prolapse, hysterectomy, removal of the ovaries, chronic pelvic pain), depression, various cancer diagnoses/treatments plus others.
- Medications: many medications can cause desire, arousal and orgasm disorders including antihistamines, amphetamines, cardiovascular and antihypertensive medicines, various hormonal preparation (especially oral contraceptives and oral oestrogens),thyroxine, narcotics and some chemotherapeutic agents. See your doctor or pharmacist for detailed information.
- Biosocial: minimal or absence of sex education/knowledge, relationship issues, history of physical, emotional and/or sexual abuse, cultural and religious customs can contribute to sexual dysfunction
Treatment Options
HSDD is TREATABLE.
Treatments can vary, so see your doctor.
Treatment options include:
Education: Many patients experience HSDD due to lack of knowledge or understanding of sexual function. Your doctor may provide advice or educational material and, if necessary, may refer you to a health care professional skilled in sexual health areas depending upon your needs.
Medication: Some medications can alter sexual motivation and responsiveness. Your doctor will review any medicines you are currently taking and may adjust these if necessary. Never change prescribed medications without first consulting your doctor.
Lifestyle changes: Lifestyle changes may need to be made in addition to other treatment options. This includes adopting a healthy diet, regular exercise, stress management, quitting smoking, and reducing your alcohol intake.
Relationships: Poor communications in a relationship can have a profound effect on sexual motivation for both partners. Counselling with your doctor or a skilled healthcare professional can often address areas of need. Solutions may be as simple as planning intimate time with your partner.
Psychological intervention: Cognitive behavioural therapy (CBT), dialectical behavioural therapy (DBT) and mindfulness therapy can all assist to varying degrees with HSDD.
Hormone therapy: Hormones, especially body-identical hormones, alone or in combination can be very effective in managing direct menopausal symptoms directly as well as treating HSDD. In Australia, there is a hormone-containing skin cream registered on the Australian Register of Therapeutic Goods (ARTG) for the management of HSDD in postmenopausal women.
Engaging your Doctor
We understand that this maybe a sensitive subject. Many women feel discomfort or embarrassment which contributes to their unwillingness to seek treatment (only 20% of women with HSDD actively consult with their doctor).
In order to facilitate discussing this subject with your physician please download and answer the Screener Questionnaire and present it to your doctor.
HSDD Screener
Doctors who are members of the Australasian Menopause Society (AMS) have a special interest in women’s health in midlife and menopause, and the promotion of healthy ageing.
To help you find a doctor who is right for you the AMS search feature Find an AMS doctor may be useful.